The FIP Development Goals are strong focus points for joint efforts of the FIP global community. I have written about vaccine availability in low- and middle-income countries (LMICs) before. This closely relates to the FIP DGs 10 (Equity and equality) and 18 (Access to medicines & services). The good news is more countries or state unions are realising that public health is not just a national affair. Vaccine donations have been pledged to support LMIC vaccine accessibility.
More close to our own Hospital Pharmacy ‘domain’, another inequity in accessibility is rolling out in front of our eyes. The good news was the WHO updated patient care guidelines for seriously ill hospitalised COVID-19 patients to include one of the few medications proven to be effective, interleukin-6 receptor blockers (IL6rb). This led to equality in care standards throughout the world. The downside is that, due to increased global demand, we are now running into supply problems for one of the IL6rbs, tocilizumab. Where HI countries are either (again) scrambling to get their own supply secured, or are able to use alternatives like sarilumab, many LMICs cannot access these or afford them. And, specifically LI are exposed to the dangers of counterfeit tocilizumab that are now being encountered. The HPS is actively taking part in the discussions to tackle the current problem of COVID-19 care and IL6rb access inequality.
The WHO links the inequitable distribution of vaccines to people in LMICs being susceptible to severe forms of COVID-19. So LMICs are doubly hit: no vaccines and no access to effective treatment. The WHO calls on manufacturers to reduce prices and make supplies available to LMICs, especially where COVID-19 is surging. WHO also encourages companies to agree to transparent, non-exclusive voluntary licensing agreements using the C-TAP platform and the Medicines Patent Pool, or to waive exclusivity rights. In addition, WHO has launched an Expression of Interest for prequalification of manufacturers of iIL6rb. Unitaid and the WHO have issued a joint statement on the IL6rb shortage. The ACT-A partnership Access to COVID-19 Tools (ACT) Accelerator partners are working with Roche to set up channels for distribution of tocilizumab in places where it is not yet in use, as part of their effort to support roll-out of effective new therapeutic products for COVID-19. With a global shortage of tocilizumab and lag times for these measures to take effect, these recommendations will not totally solve the current situation. They will however, be important lessons to learn how to be prepared for future situations that might enhance inequality in access to medicines. I hope the HPS community will continue to play a role in this field.
Kind regards,
Rob Moss, President FIP Hospital Pharmacy Section


![]()

“APOTEKER ISUN” – An App to Overcome the Limitations of Pharmacy Services
Ari Kurnianingsih, Head of Pharmacy Dept, Blambangan District Hospital, East Java, Indonesia
Pharmacists should ensure that medications are safe and work effectively as per indication. To achieve this, pharmaceutical care activities such as medication history taking, medication reconciliation, adverse effects monitoring, and patient education on medication use are required. Normally, one pharmacist can only serve up to 50 outpatients per day. However, the number of outpatients and inpatients in our hospital reaches 400 and 150 patients per day, respectively, and there are 10 pharmacists for both administration and clinical pharmacy services. Therefore, concern was raised as to whether all patients are properly informed regarding the use of their medications. Elderly patients (35% of our patients) need special attention and assistance; for example, some patients told us that they took furosemide in the evening, when it should have been taken in the morning.
Advanced information technology has arrived in all aspects of life, including the healthcare system. We believe that technology can be used to provide services according to accepted standards and this will improve patient safety. Therefore, we developed an android-based application to provide information in a personal approach, according to patients’ diseases and medications. We named the application as APOTEKER ISUN (‘My Pharmacist’).
This app was made to assist patients with medication use and to improve patient safety. In addition, the app will improve the relationship between pharmacist and patient – ultimately leading to improved quality of pharmaceutical care. The app can be accessed using an ID card number integrated with the medical record number. Healthcare professionals in the hospital can access the entire medical history of the patient, including the clinical status progress based on laboratory test results. These data are displayed in a user friendly interface in the form of a curve on a monthly basis.
APOTEKER ISUN has an “alarm” feature that spells the medication name. This is set by pharmacists when they process the prescription in the hospital information system. This feature can minimize errors or misses regarding the time of taking medications. An algorithm was applied that can automatically manage the order of taking medications on an hourly basis. Therefore, patients only need to follow the notice from the app to take their medicines. The potential risk of missing a dose will be minimized, especially for patients with many medications. Moreover, patients are helped by detailed information provided in the app. The information includes indication, how the medication works, warnings and precautions, which are all written in lay language.
APOTEKER ISUN also provides a chat feature to facilitate communication between a pharmacist and a patient who seeks information and consultation. The app also provides a feature hoax-counteract that has become common in social media recently. In the future, a pharmaceutical care feature will be added where pharmacists can prepare a tailor-made form according to the patient’s need. Challenges in clinical practice can be turned into opportunities to achieve the optimal role of the pharmacist as a trusted profession in healthcare services.

![]()
Medication Delivery Service During the COVID-19 Pandemic
Pongsri Phuawaranukhroh, Dept of Pharmacy, Ratchaphiphat Hospital, Bangkok, Thailand
Karunrat Tewthanom, Dept of Pharmacy, Silpakorn University, Nakhon Pathom, Thailand
The COVID-19 pandemic has made us find ways to provide a safe healthcare service for both patients and healthcare workers by minimizing direct contact between them. A 277-bed government owned hospital located in Bangkok, Thailand took an initiative to provide a medication delivery service for chronic disease patients, such as those with diabetes, hypertension and dyslipidemia. A multidisciplinary team was formed to design and implement this program. In the beginning, the program targeted only non-communicable diseases but has now expanded for HIV patients.
The implementation of the service for HIV patients was challenging. These patients are classified into green, yellow and red groups based on their adherence level and viral load suppression. Patients with good adherence and sufficient viral load suppression belong to the green group. The service was not attractive to the green group since they would like to see the physician to monitor their health. Therefore, telemedicine has been offered to them in parallel with medication delivery. Acceptance from the patients increased with the new, improved service.
The pharmacy department developed smart labels with a QR code. The QR code contains complete information of the medication, such as picture, package, uses and administration. The pharmacists use telephone calls to monitor patient adherence and medication therapy outcome. The service is planned to continue beyond the pandemic as it has proved safe, convenient to patients, and it avoids crowds in the hospital.

![]()
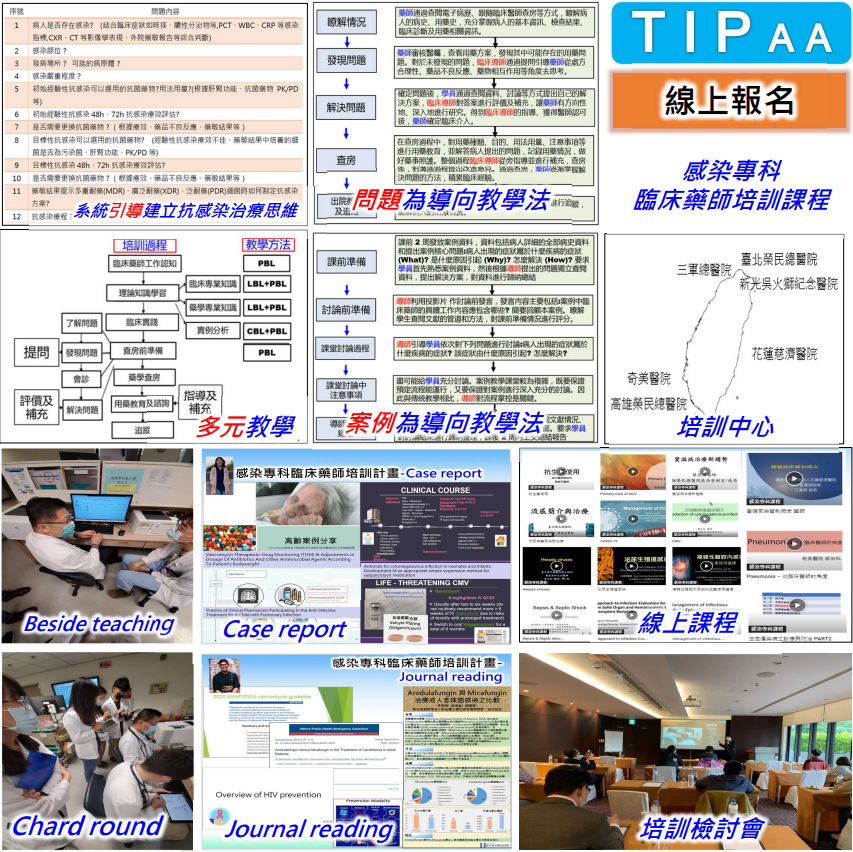
Pharmacist Community on Antimicrobial Stewardship
Fitria Nur Hidayah, RPh; Founder of APA Community
Kevin Ben Laurence, RPh; Project Management Chairperson, Asian Young Pharmacist Group
Antimicrobial resistance (AMR) is a major health concern of the World Health Organization (WHO). According to data from the Centers for Disease Control and Prevention, drug-resistant bacteria cause 23,000 deaths and 2 million illnesses annually. High levels of antimicrobial resistance pose a threat to patient safety and quality of care worldwide, including in Indonesia. The concept of one health approach presented by WHO in handling AMR problems requires the role of various healthcare professionals, one of which is the active involvement of pharmacists. This was what kickstarted the formation of the pharmacist community on antimicrobial stewardship so called APA community, “Apoteker Peduli AMR”.
“Apoteker Peduli AMR” (APA) is a community formed by the initiatives of pharmacists in several parts of Indonesia. This community is a manifestation of the joint action of pharmacists to contribute to efforts to control AMR in each practice. Since 2019, APA has played an active role in the commemoration of World Antimicrobial Awareness Week.
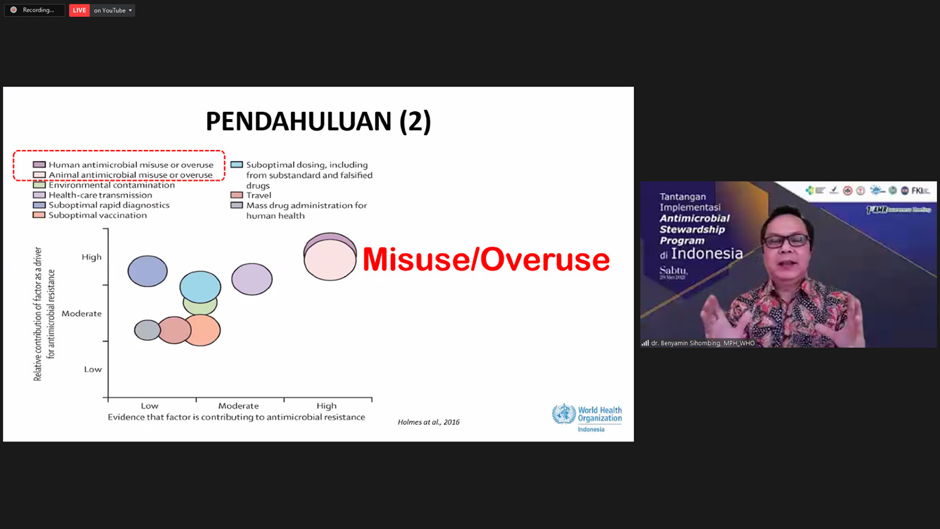
The COVID-19 pandemic provides APA with an extraordinary opportunity to collaborate in efforts to control AMR in Indonesia. The 1st AMR Awareness webinar activity with the title “Challenges of Antimicrobial Stewardship Program Implementation in Indonesia” on 29 May 2021 which was attended by 1,069 participants consisting of pharmacists, doctors, nurses and other healthcare workers is one step towards increasing awareness of the dangers of resistant antimicrobials to healthcare professionals by inviting AMR control experts from WHO Indonesia, the Indonesian Ministry of Health, the Indonesian National Agency of Drug and Food Control, health professionals, and an antimicrobial research team in Indonesia.
APA’s activities include webinars, online discussions/classes, live shows on Instagram (@apt.peduliamr), drug information campaigns, hand hygiene campaigns, APA meet friends around the world, workshops/FGDs and AMR research. Recordings of APA activities can be accessed on the “Apoteker Amrcare” YouTube channel.

![]()
Augmentation of Patient-Centered Care by Pharmacy Students as COVID Frontline Warriors
Dr. Deepak Prabhakar Bhagwat, Dept of Pharmacy, Panipat Institute of Engineering & Technology, Samalkha, Distt. Panipat
Dr. Kapil Suchal, Dept of Pharmacy, Panipat Institute of Engineering & Technology, Samalkha, Distt. Panipa
Dr. Sanjay Prabhakar Wate, Anurag College of Pharmacy, Warthi, Distt. Bhandara
Pharmacy over recent years has attained tremendous recognition as an important facet of primary healthcare and emerged as indispensable for providing need-based pharmaceutical care to a wide array of patient populations. There is a dire need for the employment of specialty pharmacists to manage a plethora of pathophysiological afflictions, viz., neurodegenerative ailments and rendering patient-centered care for special population groups, such as, pediatric, geriatric, pregnant and nursing mothers.
In today’s context, when the world is compromised in coping with the COVID-19 pandemic, there is a massive shortage of doctors and clinicians to visit rural areas and provide immediate healthcare services to alleviate and manage the symptoms of COVID-19 without further delay. Keeping this in view, the Ministry of Health and Family Welfare, Government of India has approved Clinical Pharmacists (PharmDs and M. Pharm Pharmacy Practice) to augment healthcare as COVID Frontline warriors to provide immediate pharmaceutical care and has given them the authority to dispense OTC medicines and monitor the progress of health, and to verify the side effects of drugs. Further, if the condition of the patient is seen to deteriorate, they must be sent to the nearby Government hospital without delay for hospitalization and any life support required. On July 5, after seeking approval from the Union Ministry, the Pharmacy Council of India published the gazette notification for the creation and establishment of Clinical Pharmacist posts in all Government hospitals with the definitive roles and responsibilities of clinical pharmacists in hospitals and drug-store settings, and amended the relevant Pharmacy Practice Regulations.
As a step towards further strengthening the formal role and participation of pharmacists in core healthcare activities, the Pharmacy Council of India has recently framed rules, regulations and a syllabus for running a Bachelor’s course in Pharmacy Practice alongside the existing conventional B. Pharm. course. It is a timely and visionary step for the reinforcement of healthcare services with a special focus on community service rather than catering to the needs of the pharmaceutical industry. This may prove a boon for a country of the size and population of India with over 70% habitants in rural areas. Read more here.

![]()

You’re Invited:
Join the 2021 HPS Business Meeting
All HPS members are welcomed and encouraged to join the 2021 HPS Business Meeting, to be held via zoom on Friday, 1 October 2021, 13:00-15:00 (CEST)
You will need to register for the meeting. Once you register, you will receive another link which you will use to join the meeting.
To register to attend the HPS Business Meeting, please go to:
https://us02web.zoom.us/

Call for Interest
During the HPS Business Meeting, there will be a call for interest in joining Section committees and efforts. These are great opportunities to take on an active role in the HPS! One such opportunity is as follows:
The Hospital Pharmacy Section (HPS) is searching for a new Chair of the Webinar Committee. Ideally, this individual would be willing to commit to this leadership opportunity for at least two years. This individual is required to be a member in good standing of FIP and the HPS. This role is essential to organizing informational webinars for the HPS, typically aiming for at least 4-5 webinars throughout the calendar year. In addition, the Chair will contribute to other FIP digital events not specifically organised by HPS. The Committee Chair will work with HPS Executive, Communications, Social Media, and Newsletter Committees, as well as FIP support staff to generate ideas, recruit speakers, coordinate timing, plan logistics, and promote webinar activities. There is the potential to grow the Webinar Committee to a small team based on anticipated work load and FIP HPS webinar commitments. One of the current Co-Chairs of the Webinar Committee will be available to assist in transitioning the new Chair into this position.
The HPS would like to thank Nora Gerpe, Uruguay, for her service as the recent Co-Chair of the Webinar Committee.
![]()
COVID-19 Resources
Several hospital pharmacy groups have created useful resources related to COVID-19:
EAHP: https://www.eahp.eu/hp-
ASHP: https://www.ashp.org/
RPS: https://www.rpharms.com/
SHPA: https://www.shpa.org.au/
![]()
The World has Changed: Is it Time for the Basel Statements to Change?
The first version of the Basel Statements for Hospital Pharmacy Practice was developed at the FIP Congress in Basel, Switzerland in 2008. The Statements were preceded by a global survey of hospital pharmacists representing more than 100 countries. Coordinated and led by a group of the FIP Hospital Pharmacy Section (HPS), the statements were then updated in 2014 at the FIP Congress in Bangkok, Thailand. In both 2008 and 2014, hospital pharmacists from multiple countries provided input into the development of the statements.
Over the past 18 months, healthcare across the world has seen substantial change. Many changes are likely to remain after the pandemic ends. Given all of this change, the HPS believes that we are at another point in the evolution of hospital pharmacy practice and the health care environment, and that an update could be considered. The task before us would be informed by the following steps and deliberation:
- A review of the current 2014 Statements should be done by practicing hospital pharmacists to identify additions, subtractions, or changes to address what is missing in the statements or what would be better stated in a different way. A questionnaire on the various 7 themes of the Basel Statements could facilitate identity of needed changes. Additional needs to advance hospital pharmacy practice, such as specific process steps for each statement, should be considered.
- A list of possible changes should be documented for review by all HPS members. A list of proposed changes could be posted in various HPS venues such as the HPS Newsletter and HPS social media pages to which members can comment. Open forum Zoom sessions could enable discussion. A questionnaire could facilitate the collation of comments.
- A small group of hospital pharmacists should review the comments for changes to the current Basel Statements and draft statements that respond to the gathered input.
- A draft of the revised Basel Statements should be documented and posted in the various HPS venues for review. Zoom sessions could allow for reaction to/discussion of the draft. A group of stakeholders in addition to the HPS should be invited to review and comment (e.g. Academic Pharmacy Section, FIPEd, members of BPP and BPS). A questionnaire might facilitate the collation of comments of the draft.
- A final draft of changes to the Basel Statements should be circulated to HPS members. HPS Executive Committee members should vote for approval of the draft.
- The vote should be ratified at the next HPS Business Meeting (i.e. the 2022 FIP Congress).
- Potential developers of the questionnaires suggested in the above process, steps and collation of comments could be done by members of WHoPReC, graduate students of HPS members or colleagues, grant awardees of HPS research grants, awardees of FIP Special Project grants, etc.
- Join the discussion at the HPS Business Meeting on Friday, 1 October 2021, 13:00-15:00 (CEST) to learn more about the Basel Statements and provide your input. In addition to gathering information, you will be able to express interest in participating in the work of the section to update the Basel Statements. To register to attend the HPS Business Meeting, please go to: https://us02web.zoom.us/
meeting/register/tZMsd- CtqD8jEtHrscGIUL2jP9x4-YH2dUjo . 
A Tribute to Dr. Joseph A. Oddis
Marianne Ivey, Immediate Past President, FIP Hospital Pharmacy Section
… As ASHP President, I accompanied Joe to an annual congress of the International Pharmaceutical Federation and saw firsthand the value of his graciousness, quiet strength, and listening ability in maneuvering through the politics of an international body. Later, I became quite active in FIP, especially in the leadership of the Hospital Pharmacy Section. When I received the ASHP Donald E. Francke Medal in 2017, I was happy that Joe and his daughter Marie were in the audience to hear my expression of gratitude to him for engaging me in the work of advancing pharmacy on a global level.
In recent years when I was in Washington, D.C., or at an ASHP meeting, Joe and I would have lunch together, always with warm conversations about pharmacy, family, and life. He continued to be a role model for me. Rest in peace with angels, Joe.
Click here to see the full Tribute to Dr. Joseph A Oddis, published in August 2021 in the American Journal of Health-System Pharmacy.

Dr. Oddis and ASHP Past Presidents assembled at the 1982 dedication of the Donald E. Francke Memorial Library at ASHP headquarters. Seated, L-R: George Phillips, Wendell Hill, David Zilz, Marianne Ivey, Joseph Oddis, Milton Skolaut. Standing, L-R: Robert Lantos, Arthur Dodds, Harold Godwin, John Zugich, Vernon Trygstad, Carl Lyons, George Archambault.
![]()

Save the Date
The FIP HPS are leading webinars hosted by the central FIP team. The following dates have been booked, so save the dates and follow HPS Social Media for registration links!
- Digital Health and Hospital Pharmacy
4 October 2021 at 15.00-16:30 CESTSpeakers:
José Manuel Martínez Sesmero; Hospital Clínico San Carlos (Spain)
Katherine Miller; University of Kansas Health System (USA)
Johlee Odinet; University of North Carolina Medical Center (USA)For the webinar on 4 October, the perspective will be digital health technologies useful in a professional hospital practice setting. Mhealth will be highlighted. Access to mobile phones is nearly universal, so using these phones requires no major investment for implementation at a pharmacy level. Many apps used in mHealth are free; it is hoped that this technology will be useful for both developing and underdeveloped countries.
- Role of the Hospital Pharmacist in Antimicrobial Stewardship and Sepsis Management
19 November 2021, time TBDSpeakers:
Esteban Zabaleta; Hospital Clínica Bíblica (Costa Rica)
Shu-Wen “Wendy” Lin; National Taiwan University Cancer Center (Taiwan)
Asad “Sid” Patanwala; University of Sidney (Australia)

Webinars on Demand
FIP continues to host a rich series of webinars on a variety of relevant topics! All are available in the FIP library.We think you may be particularly interested in:
- FIP “Setting goals for the decade ahead”, FIP Development Goal 19: Patient safety. (17 Sept)
- Suicide prevention, burnout and pandemics: Supporting pharmacists’ mental health and wellbeing (10 Sept)
- Optimising opioid use through pharmacists (31 Aug)
- Advanced and specialist pharmacist development for hospital pharmacists (30 Aug)
- Health illiteracy and vaccine misinformation as determinants for equity: developing policies to establish access to quality information in an equitable way (26 Aug)
- FIP “Setting goals for the decade ahead”, FIP Development Goal 7: Advancing integrated services (18 Aug)
- FIP “Setting goals for the decade ahead”, FIP Development Goal 4: Advanced and specialist development (4 Aug)
…and last but certainly not least, a recorded Webinar providing helpful tips for completing the Basel Statements Assessment Survey

![]()

Pharmacy student-assisted medication reconciliation
Workforce limitations can be a barrier to providing medication reconciliation. This study describes the number and type of medication discrepancies identified by pharmacy students when conducting best possible medication histories for patients on admission to hospital. The study included final year bachelor of pharmacy students in Australia. In total, 294 patients included in the study. Overall, 72% (n=212/294) had medication discrepancies, the most common type being drug omission. A total of 645 discrepancies were identified, which was a median of three per patient. Patients with discrepancies were older than patients without discrepancies with a median (IQR) age of 74 (65-84) vs 68 (53-77) years (p=0.001). They also took more medicines with a median (IQR) number of 9 (6-3) vs 7 (2-10) medicines per patient (p<0.001). The most common types of medicines involved were those related to the alimentary tract and cardiovascular system. Pharmacy students may provide a beneficial service to the hospital and contribute to improved patient safety by assisting pharmacists with medication reconciliation.
Access the full article here.